
How To Reverse Insulin Resistance Naturally
Insulin resistance is a hot topic these days – you may have heard of it being to linked to conditions like weight gain, blood sugar levels, menopause, hormonal imbalances, heart disease, and more.
But what it is all about?
How can you tell if you have it, and most importantly, what steps can you take to address it?
In this blog post, we’ll break down the basics of insulin resistance—what it is, what causes it, the warning signs to watch for, and practical lifestyle strategies to help you manage or even reverse it. Let’s dive in!
What Does Insulin Resistance Mean?
Insulin resistance is a metabolic condition where the cells in your body become less responsive to insulin. This leads to elevated insulin levels and, over time, increased blood sugar levels and a range of associated health issues.
It’s influenced by a number of different factors, including genetics, obesity, diet, a sedentary lifestyle, and inflammation.
But to understand insulin resistance, it helps to first understand the role of insulin itself.
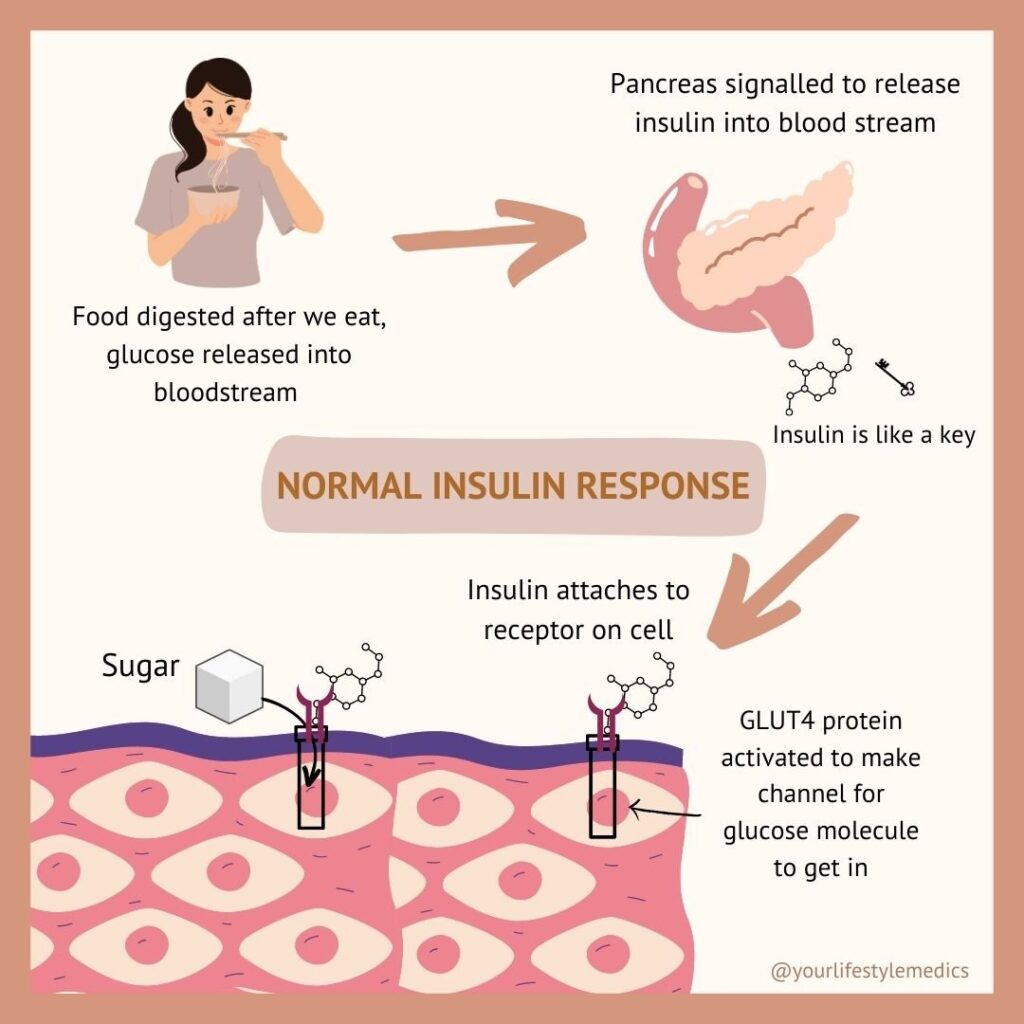
Insulin is a hormone produced by your pancreas, that helps regulate your blood sugar levels. Think of insulin as a key that unlocks cells, allowing glucose—the body’s preferred fuel—to enter from the bloodstream.
Here’s how it works:
After you eat, blood sugar rises, which signals your pancreas to release insulin. Insulin travels through your blood, and binds to receptors on the surface of your cells, activating transporter proteins called GLUT4.
These GLUT4 transporters act as channels that usher glucose inside your cells, taking it out of your blood. Your cells can use this glucose for energy immediately, or store it for later.
Once all the glucose from your meal is taken up into your cells, your blood sugar level drops down again. This signals your pancreas to stop producing insulin, while the ‘transport proteins’ move back inside the cell to wait for your next meal. This finely tuned feedback loop keeps your blood sugar within a tightly controlled range – not too high, not too low.
What Happens In Insulin Resistance
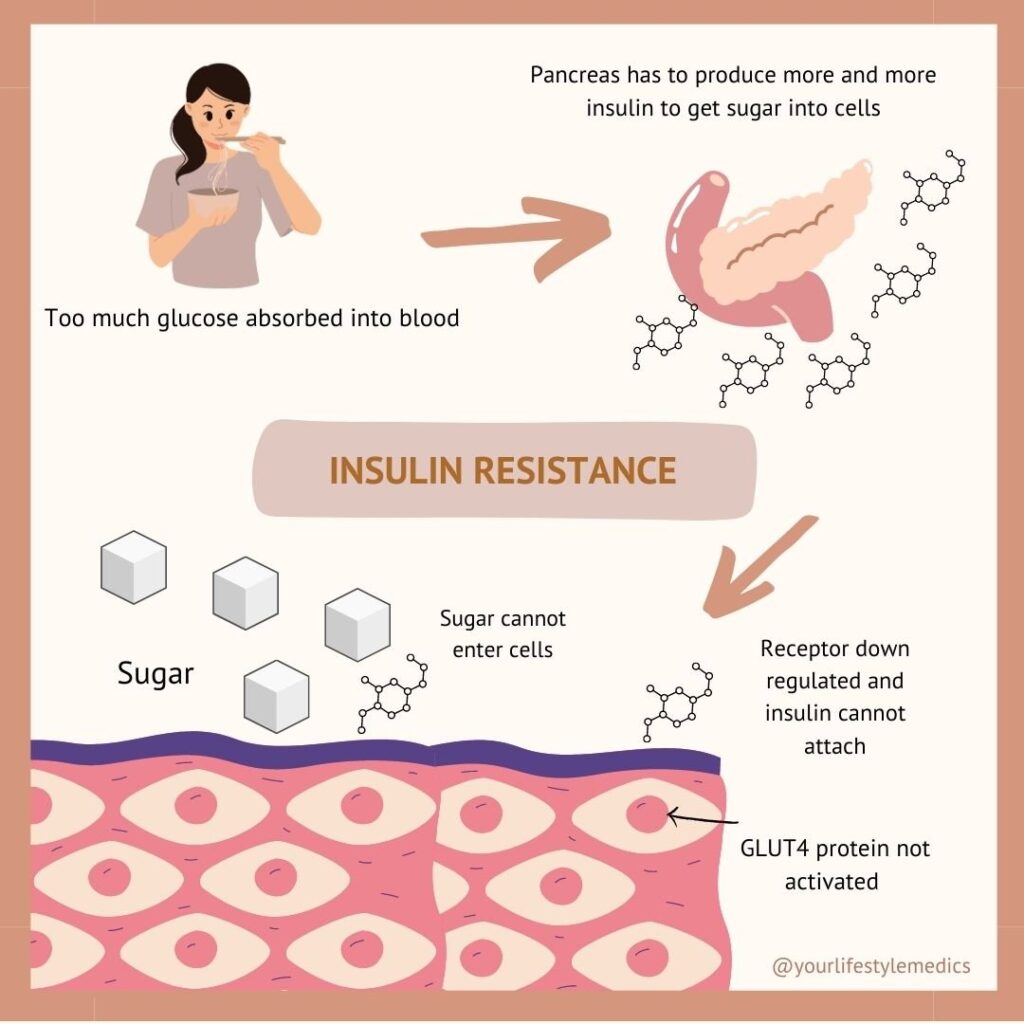
In contrast, in insulin resistance, your cells become less responsive (ie ‘resistant’) to insulin—the key fits the lock poorly or not at all.
This means glucose cannot enter the cells efficiently, causing blood sugar levels to remain high.
To compensate, your pancreas produces more insulin, sometimes leading to excessively high insulin levels (hyperinsulinemia).
This can show up initially as elevated blood sugars after meals (postprandial hyperglycemia), or blood sugar ‘crashes’ (reactive hypoglycemia).
Over time, your pancreas may eventually struggle to keep up, leading to elevated fasting glucose levels and an HbA1c that gradually increases.
This may progress to prediabetes and even type 2 diabetes in some people, and also contributes to conditions like metabolic syndrome, fatty liver disease, and heart disease.
Insulin resistance usually develops gradually over years, so recognizing early warning signs and risk factors is crucial for prevention and management.
Why Does Insulin Resistance Happen?
Insulin resistance is complex, but it arises mainly due to a combination of factors that disrupt how your body’s cells respond to insulin. These include:
- Chronic Inflammation:Low-grade inflammation interferes with insulin signaling pathways, which prevents cells from responding properly to insulin. .
- Lipid accumulation::Excess body fat (in particular visceral, or ‘tummy’ fat) stored around internal organs releases harmful substances that impair insulin function and promote more inflammation.
- Energy Surplus: Consuming more calories than the body needs leads to overfilled fat cells that become stressed and reduce the number of insulin receptors, worsening insulin resistance.
It can be useful to think of fat cells like a suitcase. Our fat cells are designed to store energy to keep us alive when food is scarce, but they have limits.
If fat cells (aka the suitcase) are filled to capacity, eventually, there’s no room left, and the suitcase won’t close – so the suitcase tries to stop more clothes coming in.
In the case of fat cells, this means they get stressed, and start to release inflammatory signals, which reduce the number of insulin receptors on their surface.
But our body doesn’t like glucose remaining in our bloodstream, as it’s highly damaging to cells – so it keeps trying harder and harder to move glucose out of our blood, by making more insulin.
This can trigger a vicious cycle: our pancreas works harder to produce more insulin, in order to try to force our cells to take up glucose, but our cells refuse to cooperate as they are already too full.
Eventually, our pancreas can’t produce enough insulin to keep up – then blood sugar levels rise, leading to prediabetes and type 2 diabetes.
Our current modern lifestyles, with too much processed food and not enough movement, is a perfect storm for creating insulin resistance, and it’s fuelling a worldwide epidemic.
But fortunately, lifestyle is also powerful in preventing and even reversing this process!

How To Tell If You Are At Risk of Insulin Resistance
Insulin resistance is influenced by a variety of factors, including genetics, lifestyle, and medical conditions.
This means it’s important to be aware of whether you may be at risk of developing it so you can be proactive in screening for it, and addressing it if there are signs you might be developing insulin resistance.
Knowledge is power!
Here’s a breakdown of the key risk factors:
1. Genetics
Some people are genetically predisposed to insulin resistance, particularly those from ethnic groups such as Māori, Pacific Island, Indian, Latin American, African, and South Asian populations.
Certain genes affect how the body processes glucose and insulin, and can increase the risk of insulin resistance and type 2 diabetes, even in people with relatively healthy lifestyles.
2. Excess Body Weight
Obesity, particularly abdominal or visceral fat, is a significant risk factor. This is because excess fat in the liver, muscles, and other tissues disrupts insulin signaling, and also promotes chronic low-grade inflammation, further worsening insulin resistance.
3. Physical Inactivity
A sedentary lifestyle can reduce insulin sensitivity. Our muscle cells use around 70–90% of the glucose in our blood; when we’re inactive, this process slows down, meaning our body doesn’t process glucose well. In contrast, regular exercise improves the uptake of glucose by muscle cells. Not surprisingly screen time is also linked with insulin resistance – with direct correlation between hours spent on screens, and risk of type 2 diabetes.
4. Diet
Diets high in processed foods, sugar, and saturated fats can promote inflammation and oxidative stress, interfering with insulin signaling.
In contrast, diets rich in whole, nutrient-dense foods can help significantly reduce risk.
While carbs often get blamed for insulin resistance, research shows that plant focused diets relatively high in complex carbohydrates (from wholegrains and legumes), actually REDUCE the risk of insulin resistance and diabetes!
5. Sleep Disturbances and Stress
Lack of sleep, especially in conditions like sleep apnea, disrupts glucose metabolism and insulin signaling, increasing the risk of insulin resistance and diabetes. Chronic stress also elevates inflammation and oxidative stress, contributing to reduced insulin sensitivity.
6. Excessive Fructose Consumption
High intake of added fructose (from processed foods, soft drinks, and syrups) is strongly linked to insulin resistance. High-fructose corn syrup, in particular, is associated with significant health risks.
This does not apply to fructose from whole foods (ie fruit), as this acts differently in the body, due to the presence of fibre and other nutrients- meaning it actually protects against insulin resistance and diabetes.
7. Altered Gut Microbiota
Imbalances in gut bacteria (dysbiosis) can lead to inflammation and are emerging as a potential contributor to insulin resistance. To learn more about the gut microbiome check out our blog post here and here
8. Health Conditions
Conditions such as polycystic ovary syndrome (PCOS), gestational diabetes, high blood pressure, non-alcoholic fatty liver disease (NAFLD), and autoimmune diseases like rheumatoid arthritis and psoriasis increase the risk of insulin resistance due to a number of different factors.
9. Medications
Long-term use of certain medications—such as steroids, some blood pressure drugs, psychiatric medications, and HIV treatments—can interfere with insulin signaling and blood sugar regulation.
10. Hormonal Disorders
Conditions like Cushing’s syndrome, acromegaly, and untreated hypothyroidism can disrupt glucose and insulin metabolism, increasing the likelihood of insulin resistance. Menopause can often reduce insulin sensitivity, as oestrogen plays an important role in energy uptake into our cells. This is one reason why that stubborn belly fat is such a common issue in women during and after menopause!

Health Conditions Caused By Insulin Resistance
Insulin resistance is also a key driver of numerous health issues, including:
1. Type 2 Diabetes
As insulin resistance progresses, the pancreas struggles to produce enough insulin to maintain normal blood sugar levels. Over time, this can lead to prediabetes and type 2 diabetes. Insulin resistance often begins decades before blood sugar levels become noticeably high.
2. Cardiovascular Disease
Elevated insulin levels and chronic inflammation associated with insulin resistance increase the risk of heart attacks and strokes. High insulin can promote fat deposits in blood vessel walls, leading to blockages and cardiovascular complications.
3. Non-Alcoholic Fatty Liver Disease (NAFLD)
Insulin resistance plays a key role in NAFLD, where excess fat builds up in the liver. This can cause inflammation, scarring, and in severe cases, cirrhosis.
4. Metabolic Syndrome
This cluster of conditions—high blood pressure, high blood sugar, increased abdominal fat, and abnormal cholesterol or triglyceride levels—significantly raises the risk of type 2 diabetes, heart disease, and stroke. Metabolic syndrome is often also used as a default marker for insulin resistance, since the two are closely linked.
5. Polycystic Ovary Syndrome (PCOS)
Insulin resistance is a key factor in PCOS, a hormonal condition affecting up to 15% of women. High insulin levels can disrupt hormone balance, leading to symptoms like irregular periods, acne, and hair changes.
6. Obesity
Insulin resistance is closely linked to obesity, particularly visceral fat around internal organs. This type of fat promotes inflammation and makes weight loss more challenging, creating a feedback loop that perpetuates insulin resistance.

Signs You May Be Suffering From Insulin Resistance
Insulin resistance often develops gradually over time and may not cause noticeable symptoms in its early stages.
Because of this, prevention is key—especially if you have risk factors for developing it. Adopting healthy lifestyle habits early on can help reduce your risk and support overall metabolic health.
Insulin resistance can manifest in various ways, particularly as it progresses. Below are some of the key signs and symptoms to look out for:
1. High Blood Sugar Levels
Insulin resistance impairs the body’s ability to regulate blood sugar, leading to elevated glucose levels. This can cause symptoms like frequent urination, increased thirst, and fatigue. Blood tests can confirm high fasting glucose levels, or an elevated HbA1C. High blood sugar levels are often a late sign of insulin resistance though, occurring further down the track – sometimes decades later.
This means relying solely on HbA1C to diagnose early insulin resistance is not reliable.
2. Stubborn Weight Gain
Insulin resistance often contributes to weight gain, particularly around the abdominal area (visceral fat).
High insulin levels promote fat storage, and a waist measurement of more than 100 cm for men or 88 cm for women can be a useful early marker of insulin resistance.
3. Difficulty Losing Weight
Paradoxically, insulin resistance can make weight loss challenging. Even with a healthy diet and regular exercise, people with insulin resistance may struggle to shed excess weight due to disrupted metabolic processes.
4. Darkened Skin Patches
Acanthosis nigricans, or dark, velvety patches of skin, may develop in areas like the neck, armpits, or groin. This is a hallmark (but relatively uncommon) symptom of insulin resistance.
5. High Blood Pressure
Insulin resistance is closely linked to high blood pressure, as both conditions share common underlying mechanisms such as inflammation and disrupted vascular function. High blood pressure also further increases the risk of cardiovascular complications.
6. Unhealthy Cholesterol Levels
Insulin resistance can result in elevated triglycerides and LDL (bad cholesterol) levels, along with reduced HDL (good cholesterol). This lipid imbalance raises the risk of heart disease and other cardiovascular conditions.
8. Metabolic Syndrome
This is strongly associated with insulin resistance and significantly increases the risk of diabetes, heart attacks, and strokes. Criteria for metabolic syndrome are having three or more of the following:
- Large waist — A waistline that measures at least 89 centimeters for women and 102 centimeters for men
- High triglyceride levels — Triglyceride cholesterol levels of 1.7 mmol/L or higher
- Reduced “good” or high-density lipoprotein (HDL) cholesterol — HDL cholesterol levels of less than 1.04 mmol/L in men, or less than 1.3 mmol/L in women
- Increased blood pressure — Average blood pressure readings of 130/85 mm Hg or higher
- Elevated fasting blood sugar — Fasting glucose of 5.6 mmol/L) or higher
If you recognize these symptoms or have risk factors for insulin resistance, it’s important to consult a healthcare provider for proper assessment and guidance.
Early intervention can make a significant difference in managing and potentially reversing insulin resistance!

What Is Metabolic Syndrome and How Is It Related to Insulin Resistance?
Metabolic syndrome is a cluster of interconnected conditions that significantly increase the risk of heart disease, stroke, and type 2 diabetes. These conditions include:
- Elevated blood sugar (hyperglycemia)
- Increased blood pressure (hypertension)
- Abdominal obesity (excess fat around the waist)
- High triglyceride levels
- Low levels of HDL (“good”) cholesterol
Insulin resistance is a key driving force behind metabolic syndrome. When your body’s cells become resistant to insulin, it disrupts the regulation of glucose and fat metabolism. This leads to the buildup of abdominal fat, abnormal cholesterol and triglyceride levels, elevated blood pressure, and increased blood sugar levels. The excess insulin (hyperinsulinemia) that accompanies insulin resistance also contributes to sodium retention and sympathetic nervous system activation, further raising blood pressure.
Because of this, insulin resistance is considered the underlying cause that links the different components of metabolic syndrome together. Understanding and addressing insulin resistance through lifestyle changes not only improves blood sugar control but also helps manage blood pressure, cholesterol, and weight, reducing your overall risk for cardiovascular disease and diabetes.

Testing for Insulin Resistance: What You Need to Know
There is no one test that can reliably test for insulin resistance, so we tend to use a combination of different markers to diagnose it.
Conventional Tests
- Fasting Blood Sugar and HbA1c: These tests detect prediabetes or diabetes, but they only identify insulin resistance at a late stage—once the pancreas struggles to produce enough insulin to regulate blood sugar. An HbA1c also only measures the average blood sugar over a 3 month period, so it cannot pick up the daily fluctuations in blood sugar levels that may occur in early insulin resistance.
- Oral Glucose Tolerance Test (OGTT): This test measures how your body responds to a sugar load. While helpful, it is time-consuming and primarily evaluates blood sugar levels, not insulin directly.
- Insulin Clamp Test: Considered the gold standard for assessing insulin sensitivity, this test is used only in research settings due to its complexity and expense.
Indirect Measures of Insulin Resistance
- Fasting insulin: this measures insulin levels in a fasted state, but for a number of reasons, is not considered reliable at diagnosing insulin resistance when used in isolation.
- HOMA-IR and QUICKI Tests: These calculations, based on fasting insulin and glucose levels, offer insights into insulin resistance and can be useful markers to look at how well your body is regulating glucose and insulin
- Triglyceride-to-HDL Ratio: This simple calculation, derived from a standard cholesterol test, can serve as an accessible marker of insulin resistance. Divide your triglyceride level by your HDL cholesterol level:
- In US units (mg/dL): A ratio below 2 is ideal; above 4 is too high.
- In European units (mmol/L): A ratio below 0.87 is ideal; above 1.74 is too high.
- CGM (continuous glucose monitor): These are wearable devices that measures glucose levels continuously through the skin, normally for a 2 week period. They can pick up very early variations in blood sugar levels, such as abnormally high or low blood sugar levels after meals. While these are not diagnostic of insulin resistance, they can be an early clue that your body is not processing glucose as effectively as it should.
If you suspect you may have insulin resistance or are at high risk due to other health conditions, it’s super important to take proactive steps to reduce your risk now.
The earlier you can make lifestyle changes to help, the more you can improve your health – managing, and potentially even reversing insulin resistance!

How To Address (And Even Reverse) Insulin Resistance
The good news is that insulin resistance responds well to lifestyle changes. Even small, consistent adjustments can lead to huge improvements over time.
If this feels overwhelming, just start with one or two manageable steps that feel most achievable for you.
Once those become habits, you can build on your progress by incorporating additional changes. Remember, lasting change happens through small, sustainable steps.
Tip #1: Swap Refined Carbohydrates for Whole Grains and Watch Your Portion Sizes
Reducing your intake of refined carbohydrates and added sugars is one of the most effective ways to address insulin resistance. It reduces the amount of insulin your pancreas needs to produce, and reduces the strain on your system.
Carbohydrates often get a bad reputation, but it’s important to distinguish between refined carbs and healthy, whole carbs.
Whole-food, plant-based diets—which are naturally rich in unrefined carbs—are shown to prevent and even reverse insulin resistance and type 2 diabetes. So, it’s not carbs themselves that are the issue, but rather the type of carbs, and whether they’re eaten in the context of a balanced diet.
Refined carbohydrates (like white flour, white rice, and processed snacks) have been stripped of fiber and nutrients during processing. As a result, they’re broken down into glucose very quickly, causing rapid blood sugar spikes and increased insulin secretion. These should be limited or avoided as much as possible if you have insulin resistance.
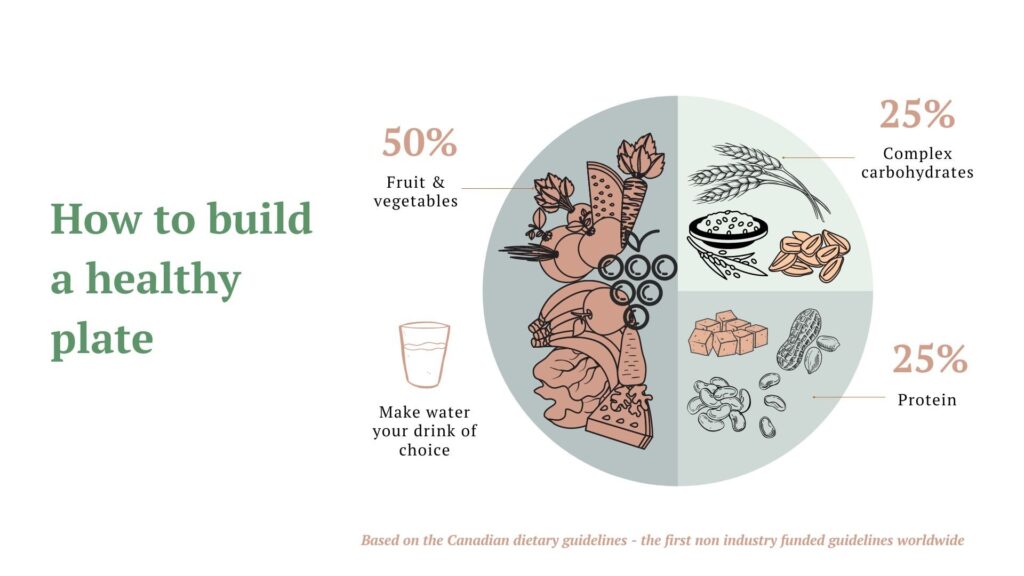
Whole grains and complex carbs (such as brown rice, quinoa, oats, legumes, fruits, and vegetables), on the other hand, are high in fiber and nutrients. These are digested more slowly, providing a steady release of glucose into the bloodstream rather than sharp spikes. They are fine to have, provided you balance them with adequate healthy proteins and fats using the guide below.
Here’s some simple tips:
- Swap white rice for brown rice or quinoa.
- Replace white bread with whole-grain bread.
- Opt for whole-wheat pasta instead of white pasta.
- Snack on whole fruits instead of sugary processed foods, refined fruit products (such as pastes), or fruit juices.
By making these small swaps, you’ll improve your blood sugar control and support better insulin sensitivity.
This is just the first step, but it’s a foundational one. For more guidance on carbs, whole grains, and insulin resistance, check out our Reboot and Nutrition Courses for in-depth support!
The graphic below shows some simple swaps, we cover carbs, whole grains and more in depth in our Reboot and Nutrition courses if you’d like to learn more.

Being mindful of your carbohydrate portion sizes is also key. It’s easy to overeat carbs, as they’re often the most convenient option. However, carbs should be just one part of your meal, not the main focus!
Aim to fill about 25% of your plate with whole carbohydrate-rich foods like grains and starchy vegetables (e.g., root vegetables), using the guide below. For a good reference, a typical serving of carbs is about 1/2 cup or one slice of bread. Even healthy foods need to be eaten in moderation!
Tip #2: Reduce or Avoid Added Sugars
Sugar can play a massive part in elevating insulin levels, as they can cause a rapid rise in glucose levels when we eat or drink them.
This is especially true for sugary foods and drinks that are low in fiber and protein, such as sodas, fruit juices, baked goods made with refined flour, ultra-processed snacks, and even many “healthy” foods like commercial cereals and granola bars.
On the other hand, when sugar is consumed as part of whole foods (like fruit), the fiber in these foods slows down the absorption of sugar, preventing those blood sugar spikes. For most people, 2-3 servings of whole fruit a day is fine, and fruit itself is actually protective against many chronic health conditions.
To reduce your sugar intake, check the nutrition label of packaged foods. Keep in mind that 4g of sugar is equal to 1 teaspoon. Ideally, women should limit added sugar to a maximum of 6 teaspoons (24g) per day, and men should stick to 9 teaspoons (36g) per day. Many packaged foods contain nearly an entire day’s worth of sugar in just one serving!
Sugar can be listed under many different names, including cane sugar, honey, maple syrup, agave nectar, dextrose, and maltodextrin. Ingredients ending in ‘-ose’ (such as fructose, glucose, maltose) are also forms of sugar.
When reading food labels, check where sugar appears in the ingredient list—ingredients are listed in order of quantity. If sugar is near the top, it’s a strong indication that the product is high in added sugars.
For more tips on reducing sugar (while still enjoying treats!), check out our article. You can also find plenty of refined-sugar-free recipes in our Reboot course, and Nutrition courses.
Tip #3: Increase Healthy Fats and Protein Intake
We like to think of this as “putting clothes on your carbs!” Healthy fats and proteins are essential for a balanced diet and can also improve insulin sensitivity. They help slow the absorption of glucose into the bloodstream, making meals more stable for your blood sugar levels.
For example, try pairing carbohydrate-rich foods like whole grains, legumes, and starchy vegetables with healthy fats such as avocados, nuts, seeds, and fatty fish. This combination will keep you full and satisfied without spiking your blood sugar. Use the healthy plate guide above for meal planning ideas.
Protein is also crucial for regulating appetite. The “protein leverage hypothesis” suggests that our bodies tend to eat until we’ve consumed enough protein, as it’s vital for survival. In simpler terms, eating enough protein at meals helps us feel full faster, reducing the likelihood of overeating or consuming excessive glucose.
You don’t need to load up on huge amounts of protein; just aim for around 1/4 of your plate to be protein rich foods – ideally mostly from plants (legumes, nuts, seeds ettc), with eggs, lean meats, or fish in moderation.
If you prefer to calculate protein requirements, aiming for 1-1.6g/kg (of lean body weight) per day is a good target – with more active people needing the higher end. For a 70kg moderately active woman this would mean 70-112g protein spread out across the day.
Research also shows that replacing animal-based proteins with plant-based proteins can improve health and longevity, so ideally aim for at least 70% of your protein to come from plant sources, like legumes, nuts, and seeds.
We have many plant protein-rich meal ideas available in our Reboot Course, and Nutrition course. Plus, we dive deep into how to balance protein, fat, and carbs for better health without restriction in our courses.

Tip #4: Move your body regularly
Exercise is one of THE most powerful tools for improving insulin sensitivity and reversing insulin resistance!
Our muscle cells absorb 70-90% of the glucose in our bloodstream, this means the more we exercise, the more glucose we use.
Regular exercise also increases the number of Glut-4 receptors in our muscle cells, which are responsible for letting glucose into cells – so more exercise means more receptors, allowing our body to take up glucose more effectively, and improving insulin sensitivity.
Muscle cells are naturally more insulin-sensitive than fat cells, meaning they need less insulin to absorb glucose from our blood. Muscles also burn more energy even at rest, which means they continue to help regulate blood sugar levels even when you’re not exercising.
Resistance training is especially beneficial because it helps store glucose more efficiently in muscle tissue, further boosting insulin sensitivity, so building muscle mass is key to combating insulin resistance.
Cardio is also important though, as during aerobic exercise, your body burns more glucose and fat for fuel, helping improve metabolism and insulin sensitivity.
Aim for at least 30 minutes of moderate-intensity exercise most days of the week, and include strength training (such as weights or resistance exercises) at least three days a week to target all muscle groups.
If finding time for a longer workout is challenging, consider “exercise snacking”—incorporating short bursts of movement throughout the day. Research shows that even this approach can be just as effective as a longer workout. For instance, a 10-minute walk after meals can reduce blood sugar levels by up to 22%, while 10 squats every hour is as effective for helping blood sugar as one 30 minute walk!
We cover exercise in depth, as well as lots of practical tips and resources to help you get moving, in our Reboot and Activity courses.

Tip #5: Get enough sleep
Sleep is essential for overall health, and getting a good night’s rest can significantly improve insulin sensitivity.
When we don’t get enough sleep, it disrupts our body’s natural circadian rhythms and increases the production of stress hormones like cortisol. Elevated cortisol levels can raise blood sugar and insulin levels, impairing insulin sensitivity.
Chronic sleep deprivation is a major risk factor for type 2 diabetes, and even one poor night’s sleep can negatively affect blood sugar and insulin levels.
Aim for 7-9 hours of quality sleep each night. If you experience symptoms such as persistent snoring, daytime fatigue, or episodes of stopped breathing while asleep, consider being screened for conditions like sleep apnea.
To learn more about the importance of sleep, how it affects your health, and practical tips for improving your sleep quality, check out our Reboot and Sleep courses.
Tip #6: Reduce Stress
Chronic stress is a hidden factor that can contribute to insulin resistance. It raises the production of stress hormones, particularly cortisol, which negatively affects insulin sensitivity.
Engaging in stress-reducing activities, such as meditation, yoga, or deep breathing exercises, can help lower stress and improve your insulin sensitivity.
In our Stress course, we cover how stress works in the body, its impact on insulin resistance, and provide practical strategies for managing stress and building resilience.
Tip #7: Consider Fasting
Intermittent fasting or time-restricted eating can be an effective strategy for reversing insulin resistance, but it’s important to approach it with caution, especially if you have a history of eating disorders, are underweight, or have specific health conditions such as pregnancy or breastfeeding.
Fasting can also be counterproductive if you’re highly stressed or short on sleep, as it can increase cortisol levels- adding fuel to the fire! If this applies to you, a safer approach is to simply reduce or avoid after dinner snacks, and have your dinner slightly early, to have an ‘eating window; rather than delaying or skipping breakfast like most fasts.
Before starting any fasting regimen, it’s also advisable to consult your doctor, especially if you are on medication or have underlying health issues.
Fasting can help lower insulin levels and promote fat breakdown for energy. It may also improve blood sugar control, which can reduce the risk of developing insulin resistance.
There’s ongoing research into various fasting approaches, such as circadian eating, time-restricted eating, fasting-mimicking diets, and intermittent calorie restriction. Time-restricted eating (for example, not eating for 12-16 hours overnight) is one of the safest and easiest methods to begin with, as it involves simply delaying breakfast and not eating after dinner. This approach has been shown to be highly effective in improving blood sugar levels.
However, fasting is not for everyone, so it’s important to listen to your body and consult with a healthcare professional before making changes.
For more information on fasting, its benefits, and how to do it safely, explore our Reboot and Nutrition courses.

Tip #8: Supplements
While we always recommend a lifestyle-first approach for improving insulin resistance (as it is the most evidence-backed and safest method), certain supplements may provide additional support. However, it’s important to note that many of the studies on these supplements are small, so the quality of evidence is still evolving.
Here are some supplements that have shown promise in improving insulin sensitivity and blood sugar control:
- Magnesium: Some studies suggest that magnesium, at a dose of 300-400 mg/day, can improve fasting blood sugar levels and support cholesterol and blood pressure levels. Many Western diets are low in magnesium, which can be found in foods such as whole grains, leafy green vegetables, legumes, and nuts. Blood tests are not generally reliable for checking magnesium levels.
- Alpha Lipoic Acid (ALA): A small study showed that taking 300 mg of ALA daily for 8 weeks significantly improved fasting and post-meal blood sugar levels. ALA is an antioxidant naturally produced by the body and found in small amounts in foods.
- Vitamin D: Research has consistently shown that vitamin D deficiency is linked to an increased risk of diabetes, and that higher vitamin D levels can reduce the risk of developing type 2 diabetes by up to 43%. Vitamin D supplementation may also improve blood sugar control, insulin sensitivity, and help regulate blood pressure, cholesterol, and inflammation. A typical dose used in trials is 4000 IU/day, but vitamin D should be monitored via blood tests, as excessive amounts can be harmful, however this is usually a non funded blood test in NZ (with some exceptions).
- Folate: Folate, a B-vitamin, may help lower blood sugar levels and improve insulin sensitivity. It also reduces homocysteine levels, an inflammatory marker associated with insulin resistance, diabetes, and cardiovascular disease. While folate supplementation can lower fasting blood sugar, it doesn’t appear to affect HbA1c levels. Folate is found in dark leafy greens, cruciferous vegetables, and legumes, making it abundant in plant-based diets. It is normally free to check on a standard blood test
- Fibre: Dietary fibre helps slow the absorption of glucose, reducing blood sugar levels. A high-fibre diet has been shown to protect against diabetes and improve blood sugar control in those with diabetes. Psyllium husk is a fibre supplement that has been shown to help improve fasting blood sugar, HbA1c, and gut health. Ideally aim for at least 30g fibre/day (the more you can tolerate the better!)
- Myo-inositol: This is a sugar polymer formed from gluocse, that can help reduce blood sugar levels and improve insulin sensitivity. Research supports it’s use in a number of health conditions including diabetes, insulin resistance, metabolic syndrome, PCOS and gestational diabetes. Inositol is made by our kidneys, however levels can be depleted by increasing age, caffeine intake, antibiotic use, sugar and refined carbohydrate intake, sodium deficiency, insulin resistance, and type 1 and type 2 diabetes. Myo-inositol is usually taken as a powder, is generally very safe to take, with recommended dosing around 2g twice a day
- Apple Cider Vinegar: Some research suggests that consuming 1-2 tablespoons of apple cider vinegar with meals can help lower blood sugar levels. It may slow stomach emptying, reducing the rate of glucose absorption, which in turn improves insulin sensitivity. One study showed that apple cider vinegar increased insulin sensitivity by 34% in insulin-resistant individuals and by 19% in those with type 2 diabetes.
- Cinnamon Cinnamon may improve insulin sensitivity and lower fasting blood sugar, by helping cells respond better to insulin, allowing glucose to be used more effectively for energy. Try adding ½ to 1 teaspoon to oatmeal, smoothies, or hot drinks to include it in your diet (it tastes good too!)
- Amla (Indian Gooseberry) Amla is a potent source of antioxidants and has been used traditionally in Ayurvedic medicine for thousands of years to support blood sugar control. Some studies suggest it can improve insulin function and lower fasting glucose levels.It comes in a powder form, which can be added to smoothies or taken as a supplement
- Berberine Berberine is a plant compound found in herbs like barberry and goldenseal, and is one of the most researched supplements for blood sugar regulation. It works by improving insulin sensitivity and reducing glucose production in the liver. It’s important to consult a healthcare provider before starting this supplement though, as it may interact with medications, and should often not be taken long-term.

YOUR ACTION PLAN FOR HEALTHY INSULIN
- Replace refined carbohydrates with high-fiber whole foods. Be aware of portion sizes
- Limit added sugars: under 6 teaspoons/day for women, 9 teaspoons/day for men. Minimise ‘liquid sugars’, ie sweet drinks. Choose mostly whole sweet foods such as whole fruit, rather than processed.
- Aim for at least 30 minutes of exercise most days, including strength training 2-3 days/week
- Prioritise 7-9 hours of quality sleep nightly.
- Use stress reduction tools like meditation or yoga.
- Track waist circumference and metabolic markers regularly.
- Consider targeted supplementation if needed
- Consult a healthcare professional for personalized advice and possible testing.
- Consider CGM use for a short period to track blood sugars in real time.
WRAPPING IT UP
We hope you’ve enjoyed this post on insulin resistance, and have learnt some useful tips to apply to your own life!
Being diagnosed with insulin resistance, prediabetes, or diabetes can come as a shock, yet there are also so many simple, evidence-based changes you can make, that will have a massive impact – both on your health and also on how well you feel.
If you need some more personalised help with your health, we offer secure telemedicine consultations NZ wide. Find out more here
Or to take a deeper dive into how to transform your health, check out our Reboot course, or Focus courses. You can also check out our other articles, which are completely free to access.
Whatever your need is, we look forward to helping you on your journey to better health, today ❤️
REFERENCES
Arner P, Rydén M. Fatty Acids, Obesity and Insulin Resistance. Obes Facts. 2015;8(2):147-55. doi: 10.1159/000381224. PMID: 25895754; PMCID: PMC5644864.
Bray GA, Bouchard C. The biology of human overfeeding: A systematic review. Obes Rev. 2020 Sep;21(9):e13040. doi: 10.1111/obr.13040. Epub 2020 Jun 8. PMID: 32515127.
Wu H, Ballantyne CM. Metabolic Inflammation and Insulin Resistance in Obesity. Circ Res. 2020 May 22;126(11):1549-1564. doi: 10.1161/CIRCRESAHA.119.315896. Epub 2020 May 21. PMID: 32437299; PMCID: PMC7250139.
Verkouter I, Noordam R, le Cessie S, van Dam RM, Lamb HJ, Rosendaal FR, van Heemst D, de Mutsert R. The Association between Adult Weight Gain and Insulin Resistance at Middle Age: Mediation by Visceral Fat and Liver Fat. J Clin Med. 2019 Sep 28;8(10):1559. doi: 10.3390/jcm8101559. PMID: 31569345; PMCID: PMC6832997.
Yu JY, Choi WJ, Lee HS, Lee JW. Relationship between inflammatory markers and visceral obesity in obese and overweight Korean adults: An observational study. Medicine (Baltimore). 2019 Mar;98(9):e14740. doi: 10.1097/MD.0000000000014740. PMID: 30817629; PMCID: PMC6831265.
Ter Horst KW, Schene MR, Holman R, Romijn JA, Serlie MJ. Effect of fructose consumption on insulin sensitivity in nondiabetic subjects: a systematic review and meta-analysis of diet-intervention trials. Am J Clin Nutr. 2016 Dec;104(6):1562-1576. doi: 10.3945/ajcn.116.137786. Epub 2016 Nov 9. PMID: 27935520.
Softic S, Stanhope KL, Boucher J, Divanovic S, Lanaspa MA, Johnson RJ, Kahn CR. Fructose and hepatic insulin resistance. Crit Rev Clin Lab Sci. 2020 Aug;57(5):308-322. doi: 10.1080/10408363.2019.1711360. Epub 2020 Jan 14. PMID: 31935149; PMCID: PMC7774304.
Keane KN, Cruzat VF, Carlessi R, de Bittencourt PI Jr, Newsholme P. Molecular Events Linking Oxidative Stress and Inflammation to Insulin Resistance and β-Cell Dysfunction. Oxid Med Cell Longev. 2015;2015:181643. doi: 10.1155/2015/181643. Epub 2015 Jul 14. PMID: 26257839; PMCID: PMC4516838.
Rehman K, Akash MS. Mechanisms of inflammatory responses and development of insulin resistance: how are they interlinked? J Biomed Sci. 2016 Dec 3;23(1):87. doi: 10.1186/s12929-016-0303-y. PMID: 27912756; PMCID: PMC5135788.
Bird SR, Hawley JA. Update on the effects of physical activity on insulin sensitivity in humans. BMJ Open Sport Exerc Med. 2017 Mar 1;2(1):e000143. doi: 10.1136/bmjsem-2016-000143. PMID: 28879026; PMCID: PMC5569266.
Lee CJ, Sears CL, Maruthur N. Gut microbiome and its role in obesity and insulin resistance. Ann N Y Acad Sci. 2020 Feb;1461(1):37-52. doi: 10.1111/nyas.14107. Epub 2019 May 14. PMID: 31087391.
Insulin Resistance & Prediabetes – NIDDK (nih.gov)
Muniyappa R, Madan R, Varghese RT. Assessing Insulin Sensitivity and Resistance in Humans. [Updated 2021 Aug 9]. In: Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK278954/
Pantoja-Torres B, Toro-Huamanchumo CJ, Urrunaga-Pastor D, Guarnizo-Poma M, Lazaro-Alcantara H, Paico-Palacios S, Del Carmen Ranilla-Seguin V, Benites-Zapata VA; Insulin Resistance and Metabolic Syndrome
Research Group. High triglycerides to HDL-cholesterol ratio is associated with insulin resistance in normal-weight healthy adults. Diabetes Metab Syndr. 2019 Jan-Feb;13(1):382-388. doi: 10.1016/j.dsx.2018.10.006. Epub 2018 Oct 10. PMID: 30641729.
Kitade H, Chen G, Ni Y, Ota T. Nonalcoholic Fatty Liver Disease and Insulin Resistance: New Insights and Potential New Treatments. Nutrients. 2017 Apr 14;9(4):387. doi: 10.3390/nu9040387. PMID: 28420094; PMCID: PMC5409726.
Moghetti P. Insulin Resistance and Polycystic Ovary Syndrome. Curr Pharm Des. 2016;22(36):5526-5534. doi: 10.2174/1381612822666160720155855. PMID: 27510482.
Munir KM, Chandrasekaran S, Gao F, Quon MJ. Mechanisms for food polyphenols to ameliorate insulin resistance and endothelial dysfunction: therapeutic implications for diabetes and its cardiovascular complications. Am J Physiol Endocrinol Metab. 2013 Sep 15;305(6):E679-86. doi: 10.1152/ajpendo.00377.2013. Epub 2013 Jul 30. PMID: 23900418; PMCID: PMC4073986.
Evert AB, et al. (2019) Nutrition Therapy for Adults with Diabetes or Prediabetes: A consensus report. DOI:
10.2337/dci19-0014
Diabetes Superstar Foods | ADA
Maruthur NM, Ma Y, Delahanty LM, Nelson JA, Aroda V, White NH, Marrero D, Brancati FL, Clark JM; Diabetes Prevention Program Research Group. Early response to preventive strategies in the Diabetes Prevention Program. J Gen Intern Med. 2013 Dec;28(12):1629-36. doi: 10.1007/s11606-013-2548-4. Epub 2013 Jul 17. PMID: 23860722; PMCID: PMC3832727.
Whillier S. Exercise and Insulin Resistance. Adv Exp Med Biol. 2020;1228:137-150. doi: 10.1007/978-981-15-1792-1_9. PMID: 32342455.
Magkos F, Tsekouras Y, Kavouras SA, Mittendorfer B, Sidossis LS. Improved insulin sensitivity after a single bout of exercise is curvilinearly related to exercise energy expenditure. Clin Sci (Lond). 2008 Jan;114(1):59-64. doi: 10.1042/CS20070134. PMID: 17635103.
Dâmaso AR, da Silveira Campos RM, Caranti DA, de Piano A, Fisberg M, Foschini D, de Lima Sanches P, Tock L, Lederman HM, Tufik S, de Mello MT. Aerobic plus resistance training was more effective in improving the visceral adiposity, metabolic profile and inflammatory markers than aerobic training in obese adolescents. J Sports Sci. 2014;32(15):1435-45. doi: 10.1080/02640414.2014.900692. Epub 2014 Apr 14. PMID: 24730354.
Suh S, Jeong IK, Kim MY, Kim YS, Shin S, Kim SS, Kim JH. Effects of resistance training and aerobic exercise on insulin sensitivity in overweight korean adolescents: a controlled randomized trial. Diabetes Metab J. 2011 Aug;35(4):418-26. doi: 10.4093/dmj.2011.35.4.418. Epub 2011 Aug 31. PMID: 21977463; PMCID: PMC3178704.
AbouAssi H, Slentz CA, Mikus CR, Tanner CJ, Bateman LA, Willis LH, Shields AT, Piner LW, Penry LE, Kraus EA, Huffman KM, Bales CW, Houmard JA, Kraus WE. The effects of aerobic, resistance, and combination training on insulin sensitivity and secretion in overweight adults from STRRIDE AT/RT: a randomized trial. J Appl Physiol (1985). 2015 Jun 15;118(12):1474-82. doi: 10.1152/japplphysiol.00509.2014. PMID: 25882384; PMCID: PMC4469920.
Reutrakul S, Van Cauter E. Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism. 2018 Jul;84:56-66. doi: 10.1016/j.metabol.2018.02.010. Epub 2018 Mar 3. PMID: 29510179.
Buxton OM, Cain SW, O’Connor SP, Porter JH, Duffy JF, Wang W, Czeisler CA, Shea SA. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci Transl Med. 2012 Apr 11;4(129):129ra43. doi: 10.1126/scitranslmed.3003200. PMID: 22496545; PMCID: PMC3678519.
Donga E, van Dijk M, van Dijk JG, Biermasz NR, Lammers GJ, van Kralingen KW, Corssmit EP, Romijn JA. A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. J Clin Endocrinol Metab. 2010 Jun;95(6):2963-8. doi: 10.1210/jc.2009-2430. Epub 2010 Apr 6. PMID: 20371664.
Yan YX, Xiao HB, Wang SS, Zhao J, He Y, Wang W, Dong J. Investigation of the Relationship Between Chronic Stress and Insulin Resistance in a Chinese Population. J Epidemiol. 2016 Jul 5;26(7):355-60. doi: 10.2188/jea.JE20150183. Epub 2016 Jan 30. PMID: 26830350; PMCID: PMC4919480.
Holmäng A, Björntorp P. The effects of cortisol on insulin sensitivity in muscle. Acta Physiol Scand. 1992 Apr;144(4):425-31. doi: 10.1111/j.1748-1716.1992.tb09316.x. PMID: 1605044.
Adam TC, Hasson RE, Ventura EE, Toledo-Corral C, Le KA, Mahurkar S, Lane CJ, Weigensberg MJ, Goran MI. Cortisol is negatively associated with insulin sensitivity in overweight Latino youth. J Clin Endocrinol Metab. 2010 Oct;95(10):4729-35. doi: 10.1210/jc.2010-0322. Epub 2010 Jul 21. PMID: 20660036; PMCID: PMC3050109.
Yuan X, Wang J, Yang S, Gao M, Cao L, Li X, Hong D, Tian S, Sun C. Effect of Intermittent Fasting Diet on Glucose and Lipid Metabolism and Insulin Resistance in Patients with Impaired Glucose and Lipid Metabolism: A Systematic Review and Meta-Analysis. Int J Endocrinol. 2022 Mar 24;2022:6999907. doi: 10.1155/2022/6999907. PMID: 35371260; PMCID: PMC8970877.
Song Y, He K, Levitan EB, Manson JE, Liu S. Effects of oral magnesium supplementation on glycaemic control in Type 2 diabetes: a meta-analysis of randomized double-blind controlled trials. Diabet Med. Oct 2006;23(10):1050-6. doi:10.1111/j.1464-5491.2006.01852.x
Verma H, Garg R. Effect of magnesium supplementation on type 2 diabetes associated cardiovascular risk factors: a systematic review and meta-analysis. J Hum Nutr Diet. Oct 2017;30(5):621-633. doi:10.1111/jhn.12454
Poh ZX, Goh KP. A current update on the use of alpha lipoic acid in the management of type 2 diabetes mellitus. Endocr Metab Immune Disord Drug Targets. Dec 2009;9(4):392-8.
Ansar H, Mazloom Z, Kazemi F, Hejazi N. Effect of alpha-lipoic acid on blood glucose, insulin resistance and glutathione peroxidase of type 2 diabetic patients. Saudi Medical Journal. Jun 2011;32(6):584-8.
Rahimlou M, Asadi M, Banaei Jahromi N, Mansoori A. Alpha-lipoic acid (ALA) supplementation effect on glycemic and inflammatory biomarkers: A Systematic Review and meta- analysis. Clin Nutr ESPEN. Aug 2019;32:16-28. doi:10.1016/j.clnesp.2019.03.015
Mitri J, Muraru MD, Pittas AG. Vitamin D and type 2 diabetes: a systematic review. Eur J Clin Nutr. Sep 2011;65(9):1005-15. doi:10.1038/ejcn.2011.118
Lee CJ, Iyer G, Liu Y, et al. The effect of vitamin D supplementation on glucose metabolism in type 2 diabetes mellitus: A systematic review and meta-analysis of intervention studies. J Diabetes Complications. Jul 2017;31(7):1115-1126. doi:10.1016/j.jdiacomp.2017.04.019
Li X, Liu Y, Zheng Y, Wang P, Zhang Y. The effect of vitamin D supplementation on glycemic control in type 2 diabetes patients: a systematic review and meta-analysis. Nutrients. Mar 19 2018;10(3)doi:10.3390/nu10030375
Jafari T, Fal
lah AA, Barani A. Effects of vitamin D on serum lipid profile in patients with type 2 diabetes: A meta-analysis of randomized controlled trials. Clin Nutr. Dec 2016;35(6):1259-1268. doi:10.1016/j.clnu.2016.03.001
Lee KJ, Lee YJ. Effects of vitamin D on blood pressure in patients with type 2 diabetes mellitus. Int J Clin Pharmacol Ther. Apr 2016;54(4):233-42. doi:10.5414/cp202493
Mousa A, Naderpoor N, Teede H, Scragg R, de Courten B. Vitamin D supplementation for improvement of chronic low-grade inflammation in patients with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Nutr Rev. May 1 2018;76(5):380-394. doi:10.1093/nutrit/nux07
Pittas AG, Kawahara T, Jorde R, Dawson-Hughes B, Vickery EM, Angellotti E, Nelson J, Trikalinos TA, Balk EM. Vitamin D and Risk for Type 2 Diabetes in People With Prediabetes : A Systematic Review and Meta-analysis of Individual Participant Data From 3 Randomized Clinical Trials. Ann Intern Med. 2023 Mar;176(3):355-363. doi: 10.7326/M22-3018. Epub 2023 Feb 7. PMID: 36745886.
Lind MV, Lauritzen L, Kristensen M, Ross AB, Eriksen JN. Effect of folate supplementation on insulin sensitivity and type 2 diabetes: a meta-analysis of randomized controlled trials. Am J Clin Nutr. Jan 1 2019;109(1):29-42. doi:10.1093/ajcn/nqy234
Zhao JV, Schooling CM, Zhao JX. The effects of folate supplementation on glucose metabolism and risk of type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Ann Epidemiol. Apr 2018;28(4):249-257.e1. doi:10.1016/j.annepidem.2018.02.001
Breneman CB, Tucker L. Dietary fibre consumption and insulin resistance – the role of body fat and physical activity. Br J Nutr. 2013 Jul 28;110(2):375-83. doi: 10.1017/S0007114512004953. Epub 2012 Dec 7. PMID: 23218116.
Post RE, Mainous AG, 3rd, King DE, Simpson KN. Dietary fiber for the treatment of type 2 diabetes mellitus: a meta-analysis. J Am Board Fam Med. Jan-Feb 2012;25(1):16-23. doi:10.3122/jabfm.2012.01.110148
Gibb RD, McRorie JW, Jr., Russell DA, Hasselblad V, D’Alessio DA. Psyllium fiber improves glycemic control proportional to loss of glycemic control: a meta-analysis of data in euglycemic subjects, patients at risk of type 2 diabetes mellitus, and patients being treated for type 2 diabetes mellitus. Am J Clin Nutr. Dec 2015;102(6):1604-14. doi:10.3945/ajcn.115.106989
Petsiou EI, Mitrou PI, Raptis SA, Dimitriadis GD. Effect and mechanisms of action of vinegar on glucose metabolism, lipid profile, and body weight. Nutr Rev. 2014 Oct;72(10):651-61. doi: 10.1111/nure.12125. Epub 2014 Aug 28. PMID: 25168916.
Carol S. Johnston, Cindy M. Kim, Amanda J. Buller; Vinegar Improves Insulin Sensitivity to a High-Carbohydrate Meal in Subjects With Insulin Resistance or Type 2 Diabetes. Diabetes Care 1 January 2004; 27 (1): 281–282. https://doi.org/10.2337/diacare.27.1.281



