What you can do for long COVID recovery part 2: exercise and fatigue
By Dr Marissa Kelaher
Welcome to part 2 of our long COVID recovery blog!
In the first post we covered what causes long COVID; who it affects; common symptoms; and how to use nutrition, stress reduction, and breathing techniques to help recovery. We also covered tips on managing brain fog, dizziness, palpitations and POTS - please check it out here if you haven't already.
In this post, we cover how to approach exercise, and ways to manage physical fatigue - both common and often distressing symptoms in long COVID.
Note : this advice is designed to be used in conjunction with medical care, and AFTER being medically cleared by your doctor. If you have severe symptoms (fatigue, headache, breathlessness, racing heart, dizziness, or confusion) then PLEASE see your doctor first to rule out other potential causes, and do not start exercise until medically cleared to do so. A physical exam, as well as potentially blood tests, an ECG, or a chest xray, or other testing may be needed depending on your symptoms
EXERCISE
Getting back into exercise can be a huge challenge with long COVID, due to tiredness, loss of muscle mass, breathlessness and palpitations. This is particularly true if you exercised to a high level pre COVID-19 and have lost a significant level of fitness.
The degree to which people are affected varies hugely, and depends also on other factors such as lung damage, pre-existing lung issues, breathlessness, energy levels, and dizziness or palpitations.
It's also a tricky and slightly controversial area, as pushing exercise too quickly can cause a crash and burn cycle, and create post exertional malaise (see below), which can trigger relapses of symptoms and even worsen fatigue.
Yet at the same time staying active during recovery will improve:
cardiorespiratory fitness ( strength of lungs, muscles, heart and circulation.)
musculoskeletal fitness (strength of skeletal muscles ie arms, legs, core)
energy levels.
wellbeing, independence and confidence.
Exercise is also shown to reduce:
anxiety or depression.
stress levels and blood pressure.
risk of falling due to poor balance, dizziness, or muscle wasting.
risk of developing other problems associated with bed rest such as chest infections, bed sores, blood clots, reduced mobility and weakness.
Rehabilitation for long COVID therefore focuses on PACED gentle exercise, either by yourself, or with an experienced physio or personal trainer, while also paying close attention to your symptoms, and not escalating activity too quickly (ie listen to your body!) .
Paced exercise means exercising within your limits, and adjusting levels based on symptoms, ability, and fatigue, rather than following a set graded plan.
Pacing and prioritising in any exercise recovery plan is absolutely vital, please see section below on fatigue for more details on how to do this.
Physiotherapists and rehabilitation specialists can often help with cardiorespiratory and musculoskeletal exercise, and many are also trained in breathing therapy, such as Bradcliff breathing, to help with breathlessness /POTS/dizziness.
Please note - if you are suffering from chest pain, palpitations, severe breathlessness, dizziness, or have been diagnosed with POTS, then please seek advice from a physiotherapist or your Dr before starting exercise, as you may need a specific adapted plan .
For self paced exercise you can start by using the BORG scale below
This scale is based on how hard your breathing feels at rest and during activity or exercise, and using it during exercise gives guidance and a greater understanding about a safe level to exercise.
The general aim is to stay at level 4-5 during exercise, and not go above this. Aiming to do small amounts of exercise more often tends to work better than occasional more intense exercise.
One other important factor to be aware of, is that going too hard too quickly can cause post exertional malaise (PEM).
This is a significant increase in physical/mental fatigue in response to exercise, and is common in long COVID.
PEM can be debilitating and cause a relapse in symptoms, so cautious pacing and paying attention to your body and symptoms is vital.
PEM can occur straight after exercise, or it can be hours or even days later. Recovery normally takes 24 hours or longer and can affect fatigue levels, concentration, sleep, and memory. It can also cause muscle/joint pains and flu like symptoms.
To avoid PEM, follow the advice in the fatigue management section on pacing of activities.
If you experience significant fatigue symptoms after exercise then we recommend:
monitoring your heart rate as you exercise and introduce new exercises, via a heart rate tracker or smart watch /fitbit. You can also check it manually by checking your pulse if you know how.
closely monitor your rate of perceived exertion using the Borg Rating of Perceived Exertion Scale
keep your heart rate at less than 60% of your maximal heart rate (to calculate, subtract your age from 220 then multiply the answer by 0.6 ie (220 - age) x 0.6 = 60% of your maximal heart rate)
We cover the health benefits of exercise, types of exercise needed for wellbeing, and different types of exercise in our Boost your Activity and Reboot courses. These also include gentle and more advanced resistance workout videos, and beginner and advanced yoga sequences.
the 5 phases of return to exercise
An exercise rehabilitation plan is usually done in five phases.
Stay at each phase until you can do it comfortably, and it doesn't flare your symptoms.
TOP TIPS:
Spend a minimum of seven days at each phase.
Drop back a phase if you have difficulty, remembering to use the BORG scale above to guide you.
Only exercise if you feel recovered from the previous day and have no return of symptoms and no new symptoms.
Choose exercises that you enjoy. You are more likely to do them and the enjoyment will also help your mental wellbeing.
Be kind to yourself - exercise that you did prior to COVID-19 may not be appropriate to your stage of recovery, even at a lower intensity. Listen to your body and be creative
Track your exercise progress using an exercise dairy.
No exercise should be painful or cause chest pain/dizziness or severe breathlessness
PHASE 1: PREPARATION FOR RETURN TO EXERCISE
Types of exercise: short gentle walks around the house or garden if able, breathing exercises covered in the stress part of this blog (part 1), gentle flexibility and stretching exercises either sitting or lying down,or chair yoga. The graphic below shows stretching exercises (reproduced from the WHO guidelines on long COVID recovery)
PHASE 2: LOW INTENSITY ACTIVITY
Types of exercise: gentle walking, light household/garden tasks, light yoga.
Light Yoga is a form of stretching, breathing control and relaxation. As it incorporates gentle resistance exercise, controlled breathing techniques, and flexibility, all at a low intensity, it can be particularly helpful for long covid recovery.
Iyengar Yoga UK have developed a COVID 19 yoga programme, downloadable from https://iyengaryoga.org.uk/covid-19-recovery-a-suggested-yoga-programme/
We also have gentle and more advanced yoga recordings in our Boost your Activity and Reboot courses, plus there are many downloadable or recorded yoga videos online.
PHASE 3: MODERATE INTENSITY AEROBIC AND STRENGTH EXERCISES
Types of exercise: Walking - introducing gentle inclines, resistance exercise such as squats, wall sits, pushups, triceps dips, planks, lunges, and sit-ups
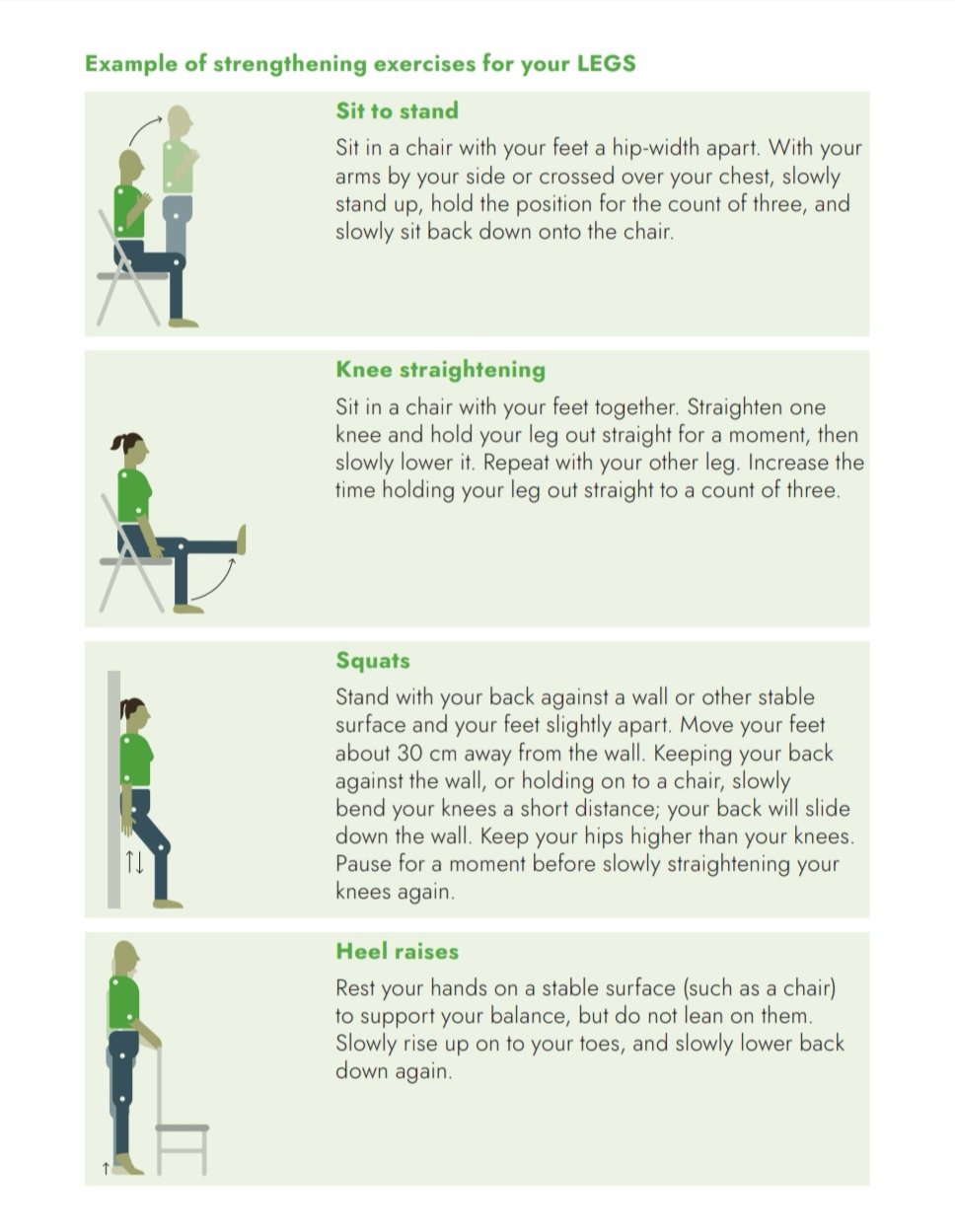
The below graphics are examples of strengthening exercises, these are reproduced from the WHO guidelines on long COVID recovery.
PHASE 4: MODERATE INTENSITY AEROBIC AND STRENGTH EXERCISES WITH CO-ORDINATION SKILLS
Types of exercise: Cycling, swimming, jogging, racket sports, zumba classes, dance classes. We have resistance, mobility, and strength training videos in our Boost your Activity and Reboot courses.
PHASE 5: RETURN TO BASELINE EXERCISE
Types of exercise: You can now return to your normal level and type of exercise.
MANAGING FATIGUE:
Fatigue is often the most debilitating part of long COVID, due to its impact on peoples ability to function and work on a daily basis. It is also one of the most common symptoms of long COVID infection.
The nutrition, stress, and exercise strategies we've gone through above can all significantly help with fatigue, as these support our body’s ability to heal and recover.
Sleep is also crucial, as its when our body and mind heal and rest, and when our brain 'cleans out' waste and unneeded information, and stores memories
For more details on how sleep works and how to improve it, please check out our sleep blog posts here and here, or for more in-depth information, our Restorative Sleep and Reboot courses. These cover how healthy sleep works, what can affect sleep, practical ways to improve sleep, plus sleep and morning meditations.
Think of your energy as a finite resource, and use the The 4 Ps method to manage it as you recover = Pace, Prioritise, Position, and Plan
pacing:
Pacing is a strategy helps you to manage activities without aggravating your symptoms.
Often it's tempting to do too much, then have to rest, then overdo it again in an attempt to catch up ('boom and bust')
Try develop an activity plan that helps you to stay within your capabilities and avoids overdoing things - listening to your body is part of this.
Breaking activities into smaller chunks and taking rests, or allowing longer to complete them can help.
Avoid activities that lead to needing a long recovery, as these can worsen symptoms.
By pacing your activities you are ensuring that:
• You are controlling the demands you place on yourself.
• These demands are within your current abilities
• You are approaching these demands in a regular controlled way, which helps to build tolerance over time.
prioritising:
When energy supplies are limited, you may need to make sure that the energy you use is spent on activities that are the most important to you. It can be helpful to prioritise what activities in your day are necessary, i.e. which tasks ‘need’ to be done, vs which ones you ‘want’ to do but aren't vital, vs what activities could be postponed to a different time or day, or which somebody else could help with.
Think of your energy as a bank machine, or an ‘energy envelope ‘ where you can withdraw a set amount each day, and choose what you want or need to spend it on. This creates a reminder to be conscious of what you spend your energy on, and helps you choose where you focus it.
Prioritising activities is very individual and what may be a priority for some may not be for others - taking time to sit and write down what things are most important to you, vs less, can help bring focus. Leave this list in a place you see often to help as a reminder.
positioning:
This is modifying activities to make them easier to perform. For example can you sit during an activity rather than standing, or have a workspace at a comfortable height with all necessary equipment within easy reach?
Things a like shower chair or bench rather than standing for showering, or other household aids are also helpful . Be creative and make it easier for yourself!
planning:
When planning your day or week, spread your activities out rather than trying to fit them all in one day, again using the concept of an energy envelope. Think about when your energy levels may be at their best (your ‘energy window’) and try doing high energy tasks at this time.
Can an activity be graded so that it doesn’t have to be done all at once? E.g. cleaning one room as opposed to the whole of the house, or doing jobs in 15 minute bursts
Creating an activity diary or a daily plan can help you pace yourself and prioritise what you want and need to do.
This is a useful downloadable one
https://movingmedicine.ac.uk/wp-content/uploads/sites/5/2021/09/COVID-workbook.pdf
You can also keep a fatigue diary each day if this helps, to track what activities make you more tired, so you can plan to pace these.
Remember - the majority of people eventually get better, and small gradual steps towards recovery is far better than trying to rush it and failing
Having honest conversations with yourself, loved ones, and your work about what you are able to manage, can help reduce feelings of pressure and stress.
If you are struggling then please reach out to your GP or local support groups, to find out what help may be available
There is a Japanese proverb that success is falling down seven times and getting up 8, which can feel very appropriate with long COVID recovery!
The key is getting up again each time when you are able, and staying focused on your long-term goals, whatever these may be ❤️
REFERENCES AND FURTHER RESOURCSE:
WHO guidelines: https://www.euro.who.int/en/countries/poland/publications/support-for-rehabilitation-self-management-after-covid-19-related-illness,-2nd-ed/docs/support-for-rehabilitation-self-management-after-covid-19-related-illness,-2nd-ed.&ved=2ahUKEwjWsKjfzfX4AhV16zgGHbIABXwQFnoECCsQAQ&usg=AOvVaw1k_4kbJYPJazVJhES5YHqT
Fatigue management guidelines: https://onlinelibrary.wiley.com/doi/10.1002/pmrj.12684
https://www.healthnavigator.org.nz/health-a-z/c/covid-19-positive-exercise/
https://longcovid.physio/
https://www.shu.ac.uk/advanced-wellbeing-research-centre/projects/an-information-booklet-to-help-manage-chronic-fatigue-brought-on-by-covid-19
https://movingmedicine.ac.uk/covidrecovery/
https://www.bmj.com/content/372/bmj.m4721
https://www.mdpi.com/1660-4601/19/9/5093
https://pubmed.ncbi.nlm.nih.gov/33923972/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8156194/